Troubleshooting Insulin Pump Problems
Dear Colleague,
I have compiled some information on the insulin infusion pump and have attached herewith.
Few useful tips:
2-Emergency paramedic / in-patient management should be according to standard iv dextrose and insulin protocols with pump therapy relinquished in the short term. Likewise all patients have been counselled to accept routine in-patient protocols for glycaemic stabilisation. If the in-patient team are happy to support the patient in managing their own pump in hospital, that is fine; but pump users are by-and-large encouraged to contact the team for advice on recommencing pump therapy prior to discharge.
3-If you need help ,the diabetes specialist nurse Emma Heslop can be contacted through DSN helpline (0191 2563003) or ext 22595 from 9 am -5 pm. Dr Shaw is more than happy to help at anytime if you contact him through switchboard (I have put these numbers in the folder as well).
A training session on CSII has been organised with Dr Shaw on 26 Jan 2007 at 2 pm in the seminar room in the Newcastle Diabetes Centre. Please inform myself or Dr Shaw if you are interested.
Arut
Arutchelvam
Clinical Research Fellow & SPR
It is important you check your glucose level a minimum of 4-6 times per day. This will help you detect any significant changes in your glucose control, so that you can respond quickly. Symptoms of hypoglycaemia may be different on a pump, so if in doubt check your glucose level.
Treatment of Low Glucose Levels:
- Take 15 grams of fast acting carbohydrate e.g. approximately 4 glucose tablets (check dose on packet for accuracy), 4 - 5 fruit pastels, 90 ml fruit juice or sugary drink. Please read the label to accurately calculate how much is needed.
- Test blood glucose level again in 15 mins
- If the glucose level is still4 mmol/l or less repeat steps above
- Always carry fast acting carbohydrate with you
Try to identify the cause and take preventative measures:
- Is the correct basal rate set?
- Has the correct bolus been given?
- Does the insulin dose relate to the carbohydrate intake?
- Check the pump’s alarm screen to see if an error has been identified
- Carry out a “self – test” if applicable to check the pump is functioning correctly
- Has more exercise been taken than usual?
- Have you been exposed to excessive heat such as sauna, bath or sun?
- Always check your glucose level before you go to bed. Confirm the appropriate levels with your health care team e.g. not below 7.0 – 8.0mmol/l for the first few days of starting pump therapy
- Avoid driving until your blood glucose levels are more predictable. Discuss the appropriate level with your healthcare team; avoid driving if your glucose level is below the recommended level. Monitor your glucose level before you drive. On long journeys repeat the glucose test at least 2 hourly.
- Monitor your glucose levels before, during and after exercise
- Carry out an extra test if alcohol has been consumed
- Make sure your family, friends, colleagues or teachers know how to treat a hypo including the administration of GlucaGen
- Show family members how to cancel the alarms and how to stop and suspend the pump
- Set the auto – off safety alarm
- Pre – set the maximum basal and bolus rates
- Consider using other features of the pump such as the bolus wizard or CarbSmart, temporary basals and different types of boluses.
Please liaise with Dr Shaw or Emma Heslop following all calls (the following morning; after the weekend; or if need additional input out-of-hours)
HYPOLGLYCAEMIA FLOWCHART
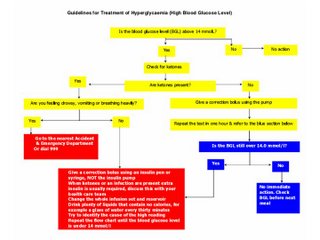
HYPERGLYCAEMIA FLOWCHART
Sick Day Rules - Coping with Illness
Your body needs insulin in order to provide glucose for the cells to create energy. Even when you do not eat, your body continues to produce glucose from your body stores. Your blood glucose level usually rises when you become ill and you will usually require more insulin. As you feel better your blood glucose level will return to your usual range. This means the insulin dose can be reduced, often to the original dose. Do not stop the insulin - you could become very ill, which may require hospital treatment.
What should you do if you are ill?
- Continue taking the insulin, do not disconnect from the pump
- Test your blood glucose level every 1 – 2 hours. Discuss with the Diabetes Team
- Take corrective insulin boluses for all glucose levels above target (eg 1 unit to reduce glucose by 2mmol/L or according to your own calculated insulin sensitivity factor or using the bolus wizard if you use this)
- Document the blood glucose results clearly
- Whilst ill aim for blood glucose levels between 5.0 to 14.0mmol/l
- Check for ketones as soon as the illness starts
- If ketones are present you may need a higher corrective dose than usual to lower your blood glucose
- Drink 3-4 litres (4-6 pints) of sugar-free liquid throughout the day
- If you do not feel like eating, replace your solid food with a sugary drink e.g. sipping lucozade, milk, fruit juice, and coke….
- If your blood glucose levels are over 14.0 mmol/l consider increasing the insulin dose (basal, bolus or by injection)
- To cope with illness you will often have to increase your basal rates by 10-20%. This can be achieved with the temporary basal feature or by reprogramming basal rates.
- Read the guidelines for the treatment of hyperglycaemia
- Y0u have ketones
- You are vomiting or too nauseated to eat or drink
- Your blood glucose level remains above 14.0 mmol/l
- Your condition does not improve
- If you are not sure what action to take
Pump contact numbers-Newcastle insulin pump service
24 hour on-call SpR/Consultant: 0191 233 6161Monday - Friday
Dr James Shaw: 0191 233 6161
Emma Heslop: 0191 233 6161 ext 22595
DSN helplin: 0191 256 3003
Editor's note: Please refer to emailed attachments for insulin dose calculation/adjustment


0 Comments:
Post a Comment
<< Home